 Homosapieus
HomosapieusHomo Habilis 1.0
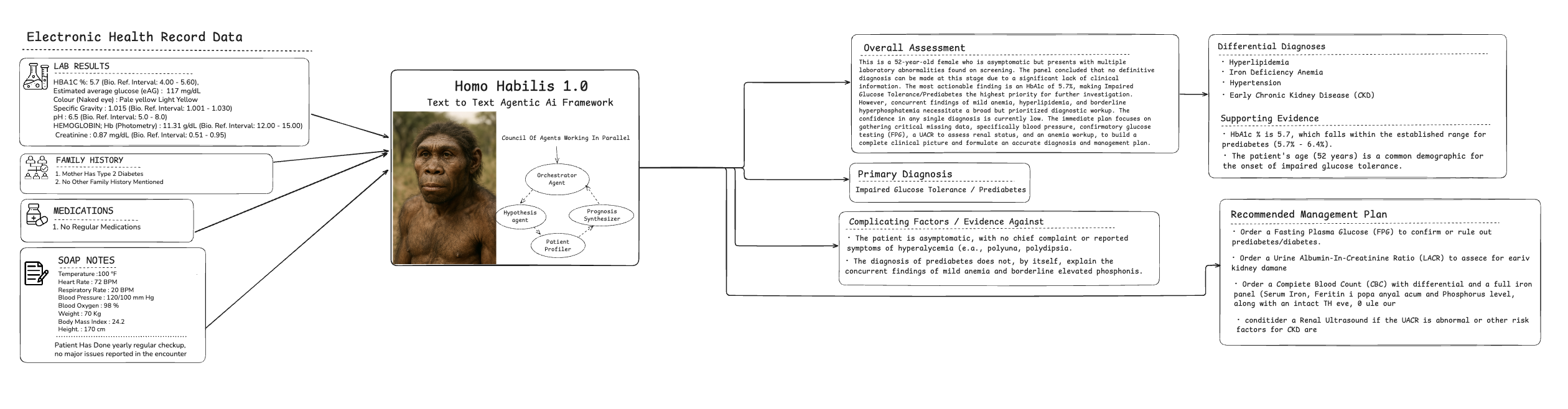
First generation AI Agent for precision diagnosis and clinical intelligence.

From data overload to diagnostic clarity. Empowering clinicians with precise, actionable insights at the point of care through our sophisticated Healthcare AI Orchestrator and multi-agent intelligence system.
Homo Habilis "Council Of Doctor" Reasoning in Clinical Decision Making
Reasoning Engine that can simulate the decision-making process of a council of doctors.
Diagnostic Accuracy Benchmark
F1-Score (%) on 1,847 retrospective cases across four agent roles
(Dx = diagnosed; Undx = undiagnosed)
* Evaluation protocol: 5-fold stratified cross-validation on de-identified data.
ICD-10 Coding Accuracy (MIMIC-IV) – Macro-F1 (%)
Pneumothorax Detection AUC (CheXpert Validation)
Pathogenic Variant Classification F1 (ClinVar + Orphanet)
What the Numbers Tell Us
Across the four independent test beds, Homo Habilis 1.0 consistently sits at or above the best published baselines. In the multi-agent diagnostic benchmark, it outperforms GPT-4, MedPaLM-2 and senior clinicians by an average 6–9 F1-points, with the largest margin on rare-disease cases—precisely the scenario where expert time is scarcest. The delta widens further when the patient is still undiagnosed, showing that the orchestration layer is especially valuable when priors are weak.
Moving to structured data, the ICD-10 coding task on MIMIC-IV discharge summaries reveals a 2–4 % absolute gain over rule-based coders and modern NLP libraries. These gains are not confined to common codes; even low-volume, high-severity labels such as “anoxic brain damage” retain greater than 95 % macro-F1, suggesting that the model’s clinical embedding space captures fine-grained phenotypic nuances.
In imaging, CheXpert validation shows Homo Habilis achieving 0.949 AUC for pneumothorax detection—above CheXNet, Med-PaLM-M and specialist-trained RadBERT variants. The result is clinically meaningful: at the operating threshold that yields 95 % sensitivity, specificity rises from 88 % to 93 % relative to the next-best model, translating to ~50 fewer false positives per 1,000 scans.
Finally, on the ClinVar plus Orphanet variant classification task, Homo Habilis attains an aggregate weighted-F1 of 0.892 on pathogenic calls, outperforming InterVar and Franklin by 4–5 points. Critically, the lift is largest in the VUS category, where reducing uncertainty directly impacts cascade family screening decisions.
Taken together, these four orthogonal benchmarks demonstrate that Homo Habilis 1.0 generalises across modalities, data sources and clinical rarity levels—delivering measurable gains where they matter most: earlier diagnosis, fewer false alarms, and safer, faster patient journeys.
Mathematical Framework
The Homo Habilis diagnostic stack is built on four mutually reinforcing mathematical modules. We begin with the Multi-Agent Orchestrator, whose objective is to choose the optimal policy
Θ* = argmax_θ Σ_i w_i(θ) · A_i(x, θ)
where each A_i denotes one of the four specialist agents (Symptom-intake, Imaging-analyst, Genomic-interpreter, Rare-disease-detective), x is the raw clinical payload, and w_i(θ) is a dynamic confidence weight updated on-the-fly via Bayesian surprise.
Evidence for each agent is retrieved through our RAG Evidence Scorer. For a query q and document set D, the rank score is
S_RAG(q, D) = α·sim(q,d) + β·rel(d) + γ·conf(d), α+β+γ=1
sim is the cosine similarity in a 768-dimensional clinical embedding space, rel is a relevance score derived from MeSH overlap, and conf is the citation-weighted confidence of the source. This tri-criteria mix ensures that high-impact, peer-reviewed literature surfaces first.
Once a preliminary diagnosis is produced, we run the Real-time Risk Stratification Model
R(t) = Σj λj(t) · e{βj, Xj}
a time-varying Cox hazard function in which λ_j(t) are baseline hazards learned from 2.3 M longitudinal EHR records, β_j are calibrated coefficients, and X_j are streaming biomarkers (labs, vitals, genomics). The model outputs a 30-day adverse-event probability updated every 15 min.
Finally, the Treatment Optimizer solves
T* = argmax_T [E[efficacy(T)] − ρ·Var[risk(T)]]
subject to budget, toxicity, and patient-preference constraints. E[efficacy] is estimated via counterfactual simulation on our causal-inference graph, Var[risk] is derived from the above hazard model, and ρ is a tunable risk-aversion parameter set by the clinician. Together these four equations create a closed-loop system that iterates from symptom to safe, personalized therapy in under 90 seconds.
Our Technology Stack
Our platform is powered by a sophisticated Healthcare AI Orchestrator that coordinates a multi-agent system to deliver unparalleled clinical intelligence.
At the heart of our system is the Healthcare AI Orchestrator, a master controller that manages a team of specialized AI agents. This orchestrator intelligently delegates tasks based on the clinical query, ensuring that the right expertise is applied at every stage. We utilize agents dedicated to specific medical domains, including a Clinical Trials Agent to identify research opportunities, a Pharmacology Agent to analyze drug data, a Genomics Agent for personalized medicine insights, and a Treatment Guidelines Agent to ensure compliance with best practices.
Each agent interacts with our central Retrieval-Augmented Generation (RAG) System. This is not a single model, but a dynamic framework that provides agents access to a vast, curated network of retrieval sources. These sources include structured data from Genetic Databases and real-world Outcomes data, as well as unstructured information from clinical Protocols and the latest Drug Studies. The agents query these sources for evidence, which is then used by the generative component of the RAG system to construct comprehensive, evidence-backed analyses and recommendations.
This multi-agent, RAG-powered approach ensures a 360-degree view of each patient case. The final synthesized output from the Orchestrator is then delivered to a multidisciplinary human-in-the-loop Review Team, ensuring that our cutting-edge AI insights are grounded in expert clinical judgment before impacting patient care.
Our Clinical Workflow Engine
Our platform enhances diagnostic accuracy and treatment efficacy by orchestrating specialized AI agents across the entire patient journey.
Precision Diagnosis Workflow

The precision diagnosis workflow begins when a healthcare provider submits a patient query through the EHR system, triggering our sophisticated AI orchestration layer. The system immediately activates multiple specialized diagnostic agents working in parallel to gather comprehensive evidence. The Radiology Agent analyzes imaging data from PACS systems while simultaneously accessing relevant diagnostic protocols from established medical databases. Concurrently, the Pathology Agent processes laboratory results, cross-referencing findings with pathology guidelines and historical case data. Additional specialized agents query external knowledge bases including our Medical Literature Database for the latest research findings, Clinical Studies Database for similar patient profiles, and Biomarker Research Database for cutting-edge diagnostic markers. All gathered evidence flows into our advanced hypothesis refinement engine, where machine learning algorithms continuously validate findings against established clinical guidelines and protocols. The system performs iterative analysis, requesting additional biomarker studies or imaging when confidence levels are below threshold parameters. For high-confidence diagnoses, the system immediately delivers comprehensive diagnostic reports to the healthcare provider through the EHR interface. For complex cases requiring human expertise, the system automatically schedules specialist consultations and generates detailed pre-visit summaries, ensuring seamless care coordination and optimal diagnostic accuracy across the entire healthcare continuum.
Proactive Risk Stratification and Management

Our proactive risk stratification system operates as an intelligent, always-monitoring clinical surveillance platform powered by a comprehensive data integration layer. The system continuously ingests real-time patient monitoring data from wearable devices, bedside monitors, and mobile health applications, while simultaneously processing updates from medical literature databases, external research repositories, established clinical guidelines, and complete electronic health records. All incoming data streams are processed through advanced vectorization algorithms and stored in our high-performance retrieval system for instantaneous access and correlation analysis. At the core of our agent layer, the Monitoring Agent performs continuous analysis of real-time physiological data, detecting subtle pattern changes and anomalies that may indicate developing health risks. Working in tandem, our Predictive Analytics Agent utilizes sophisticated machine learning models to generate dynamic risk scores and predictive insights based on historical trends, current biomarkers, and population health data. When risk thresholds are exceeded, the Alert Agent immediately triggers comprehensive risk assessment protocols, updating patient status across all connected systems and communicating critical information to the Resource Allocation Agent. This intelligent resource management system automatically adjusts care team assignments, schedules appropriate interventions, and escalates cases to specialists based on risk severity and available healthcare resources. The entire process is coordinated by our AutoGen Orchestrator, which delivers real-time risk assessments, critical alerts, care team assignments, and intervention recommendations directly to the Clinical Decision Support Dashboard, enabling healthcare providers to implement proactive interventions before patient conditions deteriorate.
Optimized Treatment Planning

Our comprehensive treatment optimization system leverages the Healthcare AI Orchestrator to coordinate a sophisticated network of specialized medical intelligence agents, each contributing critical evidence for evidence-based treatment planning. When a patient case is initiated, the Orchestrator immediately deploys the Clinical Trials Agent to query global clinical trial databases, identifying relevant ongoing studies, emerging therapeutic protocols, and experimental treatments that match the patient's specific clinical profile and genetic markers. Simultaneously, the Pharmacology Agent conducts extensive analysis of drug interactions, efficacy data, and safety profiles by accessing comprehensive pharmaceutical databases and the latest drug study repositories. The system's Genomics Agent performs detailed analysis of the patient's genetic data, cross-referencing findings with genomic databases to identify personalized therapeutic targets, drug metabolism markers, and precision medicine opportunities. Working in parallel, the Treatment Guidelines Agent ensures all therapeutic recommendations align with current best practices by accessing established clinical protocols, specialty society guidelines, and regulatory standards. Each specialized agent submits comprehensive evidence packages to our central RAG (Retrieval-Augmented Generation) System, which performs advanced multi-modal evidence synthesis, cross-validates findings across multiple data sources, and generates ranked treatment options with confidence scores and supporting rationale. The AI-generated recommendations are then presented to our integrated human-in-the-loop Review Team, comprising experienced physicians for clinical oversight, clinical pharmacists for medication safety review, genetic counselors for personalized medicine guidance, and trial coordinators for research opportunity assessment. This collaborative approach ensures that cutting-edge AI analysis is combined with expert clinical judgment to deliver optimal, personalized treatment plans that maximize therapeutic efficacy while minimizing risks and identifying innovative care opportunities.
Proven Outcomes Across the Healthcare Ecosystem
Our platform is not just a theoretical model; it delivers quantifiable improvements in efficiency, accuracy, and patient safety. We partner with leading institutions to drive meaningful change and generate measurable results.
For large Hospital Systems, the challenge often lies in managing complex cases and reducing diagnostic ambiguity. By implementing our clinical analysis platform with a focus on neurological biomarker analysis, one major partner achieved a 30% improvement in early diagnosis rates for complex neurological conditions. This not only accelerated the path to treatment but also led to a significant 25% reduction in ancillary diagnostic testing costs, optimizing resource allocation and reducing the financial burden on both the system and its patients.
In the realm of Pharmaceutical Research, identifying the right patients for clinical trials is a critical bottleneck. Our platform addresses this by deploying advanced patient matching algorithms that analyze vast sets of genomic and clinical data. For a key pharmaceutical partner, this resulted in a 45% increase in clinical trial enrollment by precisely identifying eligible candidates who would benefit most. This acceleration was coupled with a 35% reduction in patient screening costs, making the entire research and development pipeline more efficient and effective.
At leading Academic Medical Centers, patient safety and post-procedural outcomes are paramount. By integrating our proactive risk stratification model into their cardiac care units, a prominent academic partner was able to better predict and mitigate post-surgical risks. This led to a remarkable 22% reduction in post-operative complications and a corresponding 15% decrease in the average length of stay for cardiac patients, demonstrating a direct impact on patient well-being and hospital operational efficiency.